Case Law Details
Rajendra Prasad Rai Vs United India Insurance Co. Ltd. (NCDRC)
Conclusion: In present facts of the case, it was held that the Consumer was entitled to get his claim covered under the sub clause of the Insurance Policy which provides him a higher benefit.
Facts: In present facts of the case, the Revision Petition has been filed by the Petitioner against Respondents under section 21 (b) of Consumer Protection Act 1986, against the order dated 26.03.2018 of the State Consumer Disputes Redressal Commission Bihar.
The Petitioner has taken Personal Accident Policy in the year 1991-92 for insured amount of Rs.2,00,000/-. As per terms of the policy, if a premium was paid within time every year, Rs.10,000/- was to be added in sum assured every year. On 25.05.2005, i.e. during the subsistence of the insurance policy, the complainant met with an accident and was admitted in the hospital. The said information was brought to the notice of the Respondent on 26.05.2005 and FIR was also lodged. The Petitioner vide his letter dated 25.08.2005 submitted the claim with the Insurance Company. The complainant alleged that even though all the papers along with the claim were submitted for action, the Insurance Company closed the case of the Petitioner as ‘no claim’. He again resubmitted his papers and after sending reminders, legal notice, the Insurance Company sent a settlement intimation voucher asking him to receive Rs. 1,50,000/- as full and final payment. The Petitioner protested this and on being protested, the Respondent informed him that since he had opted for Table-III of the policy, therefore, he is not entitled for an amount more than Rs.1,50,000/-. It was alleged that he had opted for Table-IV of the policy and been paying the annual premium regarding the same. The Petitioner asked for other documents under RTI but the same were not supplied. He sent legal notice on 13.05.2009 and Respondent replied on 16.06.2009 stating that his claim is not maintainable and sent intimation voucher.
Petitioner approached the District Forum, wherein Complaint was partially allowed and directed the Respondents to pay Rs.1,50,000/- within 45 days from the receipt of the order failing which the Respondent would be liable to pay additional 10% annual interest on the principal amount of Rs.1,50,000/- from the date of judgment till date of payment to the Complainant. Aggrieved by the said Order dated 17.01.2017 of District Forum, Petitioners appealed in State Commission and the State Commission vide order dated 26.03.2018 in FA No. 54 of 2017 partly allowed the Appeal of Complainant and directed the Respondent to pay compensation and litigation cost and interest and allowed benefit amount of Rs.1,50,000/- with 9% p.a. from the date of filing complaint i.e. 04.12.2014, compensation of Rs.10,000/- and litigation cost of Rs.5000/-.
Petitioner challenged the said Order dated 26.03.2018 of the State Commission before the National Commission, wherein after taking submissions of both sides into consideration it was observed by the Commission that the Petitioner has admitted that he has been paid / offered settlement of claim for Rs.1.20 lacs under clause / sub clause ( e ) along with medical expenses under extended medical benefit opted. Now, the question arises, whether even under the old policy, before its restructuring in 2002, Petitioner was entitled to benefits under multiple sub clause from (a ) to ( f) or only under one of the clause from ( a) to ( f) in view of exception no.1.
Further, it was observed that in view of the exception clauses, Petitioner was not entitled to benefits under multiple sub clauses. As his claim under clause / sub clause ( e) has been accepted, he cannot make additional claim under sub clause (f) due to exception clause. However, the Complainant is to be given benefit of only one clause / sub clause, even though his case is covered under multiple clauses, he has a right to get his claim covered under the sub clause which gives him a higher benefit. Hence, although he cannot claim benefit under both sub clauses ( e) and ( f), but the Petitioner has right to choose the sub clause which gives him the higher benefit. As clause / sub clause ( e) gives him a benefit of Rs.1.20 lacs but clause ( f) gives him a benefit of Rs.2.61 lacs.
Reliance was made upon the Judgment of the Hon’ble Supreme Court in Canara Bank Vs. United India Insurance Co. Ltd. & Ors. (2020) 3 SCC 455, wherein it was observed that ‘Insurance Policy must be read holistically so as to give effect to reasonable expectations of all the parties including the insured and the beneficiaries- it must be interpreted in a commercially sensible manner-coverage clauses to be read broadly, and ambiguity, if any, to be resolved in favour of insured-exclusions to be read narrowly.”.
On basis of the above, Petitioner was entitled to claim of Rs.2.61 lacs under the policy in place of Rs.1.20 lacs, along with interest and with medical expenses under extended medical benefits (Rs.30,000/-). Hence, the State Commission’s / District Forum’s orders was modified.
FULL TEXT OF THE ORDER OF NATIONAL CONSUMER DISPUTES REDRESSAL COMMISSION NEW DELHI
1. The present Revision Petition (RP) has been filed by the Petitioner against Respondents as detailed above, under section 21 (b) of Consumer Protection Act 1986, against the order dated 26.03.2018 of the State Consumer Disputes Redressal Commission Bihar (hereinafter referred to as the ‘State Commission’), in First Appeal (FA) No. 54 of 2017 in which order dated 17.01.2017 of District Consumer Disputes Redressal Forum Hajipur (hereinafter referred to as District Forum) in Consumer Complaint (CC) no 100 of 2014 was challenged, inter alia praying for allowing the RP by allowing the prayer of the Complainant / Petitioner as prayed in CC No. 100 of 2014 before the District Forum.
2. While the Revision Petitioner (hereinafter also referred to as Complainant) was Appellant and the Respondents (hereinafter also referred to as OPs were Respondents in the said FA No. 54 of 2017 before the State Commission, the Revision Petitioner was Complainant and Respondents were OPs before the District Commission in the CC no. 100 of 2014.
3. Notice was issued to the Respondents on 06.09.2018. Parties file their Written Arguments / Synopsis on 22.02.2023 and 28.06.2023 respectively. IA No. 16657 of 2018 seeking condonation of delay of 10 days in filing the RP is allowed on account of reasons stated therein.
4. Brief facts of the case, as emerged from the RP, Order of the State Commission, Order of the District Commission and other case records are that Complainant had taken Personal Accident Policy from the OPs in the year 1991-92 for insured amount of Rs.2,00,000/-. As per the terms of the policy, if a premium was paid within time every year, Rs.10,000/- was to be added in sum assured every year. The complainant continued paying the premium till 2004-06. . On 25.05.2005, i.e. during the subsistence of the insurance policy, the complainant met with an accident and was admitted in the hospital. The said information was brought to the notice of the Opposite Party on 26.05.2005 and FIR was also lodged under section 342, 323, 324, 384, 307 and 34 of the IPC. The Petitioner vide his letter dated 25.08.2005 submitted the claim form with the Insurance Company. The complainant alleged that even though all the papers along with the claim form were submitted for action, the Insurance Company closed the case of the Complainant as ‘no claim’. He again resubmitted his papers and after sending reminders, legal notice, the Insurance Company sent a settlement intimation voucher asking him to receive R s.1,50,000/- as full and final payment. The Complainant protested this and on being protested, the opposite party informed him that since he had opted for Table-III of the policy, therefore, he is not entitled for an amount more than Rs.1,50,000/-. It is alleged by the complainant that he had opted for Table-IV of the policy and been paying the annual premium regarding the same. For this, the petitioner sought certain information from the Insurance Company and he was directed to deposit the cost for the same and the receipts were served upon him from which it was transpired that he had deposited the premium for Table IV option. The petitioner was served with one form in the year 1995-96 from which it transpired that his option for schedule IV filled up in the form was crossed and in the form itself it was written with full cover and inspite of this OPs tried to show that he had opted for Table-III. The Petitioner asked for other documents under RTI but the same were not supplied. He sent legal notice on 13.05.2009 and OPs replied on 16.06.2009 stating that his claim is not maintainable and sent intimation voucher. Petitioner alleged that OPs dishonestly and fraudulent manipulated option given by him for Table-IV by cutting the same and had written the word ‘Table-III’ in appropriate place. Being aggrieved, the petitioner initially approached the Hon’ble High Court of Patna by way of writ application bearing CWJC No. 14566 of 2009 which was disposed of on 14.11.2014 with a direction to approach the concerned consumer forum. Accordingly, Complainant filed a CC before the District Forum. Vide Order dated 17.01.2017 in the CC no. 100 of 2014 the District Forum has partially allowed the Complaint and directed the OPs to pay Rs.1,50,000/- to the Complainant within 45 days from the receipt of the order failing which the OPs will be liable to pay additional 10% annual interest on the principal amount of Rs.1,50,000/- from the date of judgment till date of payment to the Complainant. Aggrieved by the said Order dated 17.01.2017 of District Forum, Petitioners appealed in State Commission and the State Commission vide order dated 26.03.2018 in FA No. 54 of 2017 partly allowed the Appeal of Complainant and directed the OPs to pay compensation and litigation cost and interest and allowed benefit amount of Rs.1,50,000/- with 9% p.a. from the date of filing complaint i.e. 04.12.2014, compensation of Rs.10,000/- and litigation cost of Rs.5000/-. It further directed that amount be paid within two months from the receipt of the order failing which 12% will be payable. Hence the Complainant is before this Commission now in the present RP.
5. Petitioner has challenged the said Order dated 26.03.2018 of the State Commission mainly/inter alia on following grounds:
i. The State Commission did not consider the terms and conditions of the policy issued to the Petitioner as the Petitioner is entitled for the following benefits:
a. 40% of the Capital Sum Insured ( CSI) ( including Cumulative Bonus ( CB) ) under sub-clause e (xii) of the policy ( corresponding to benefits No.5 read with entry No. xii in the old policy) since the petitioner has suffered 40% permanent partial disablement 40% of Rs.3,00,000/- = Rs. 1,20,000/-.
b. Under sub-clause ( f ) of the policy ( corresponding to benefit No.6 of the old policy) : 1% of the CSI ( including CB) for 87 weeks ( the actual period the petitioner was totally disabled from engaging the employment) since 1 % of the CSI Rs.3009 x 87 = Rs.2,61,000/-.
c. Medical expenses under extended medical benefit opted by the petitioner by paying 10% additional premium every year, amount to 10% of the CSI ( including CB) 10% of Rs.3,00,000/- = Rs.30000/-
d. Therefore, the total entitlement of the petitioner was Rs.3,00,000/- ( mentioned as (a ) and (b) above capped to CSI) + Rs.30000/- ( medical benefits mentioned at (c) above) amounting to a total of Rs.330000/- as payable to the petitioner in month of June, 2005.
(ii) State Commission ought to have considered the malafide act and fraudulent rejection of the claim by the OPs on the false plea that under sub clause (f) corresponding to benefit no. 6 of the policy deed on the ground Petitioner is not entitled to benefit no. 6 as he has taken the policy under Table-III , whereas perusal of policy deed of the petitioner for the year 1996-97 and 1997-98 shows that at the time of taking of the policy by the petitioner table III was the top most option available and it included all the benefits and petitioner has opted for the same.
(iii) The State Commission should have considered the policy in actual term and terms of the original policy based on which the petitioner had renewed the policy.
(iv) The Respondents have subsequently restructured the said scheme and instead of 3 tables in total, they have divided the scheme in 4 different tables wherein the benefits opted for and paid by the petitioner ( i.e. benefit No. 1 to 6 ) have been put under the newly formed Table IV.
(v) No intimation or consent was obtained at the time renewal of the policy regarding any change and Petitioner has never been asked for any of his opinion or option regarding the same and he had been paying the premium according to his initial option of the benefits ( benefit no. 1 to 6 ).
(vi) The Petitioner was not provided even with the part payment of the claim amount or the amount admitted by the respondents are payable and that Petitioner was blackmailed by the respondents to sign a declaration to the effect that no further claim of the petitioner would remain due with the respondents if he would take the said admitted amount as part payment of the claim.
6 Heard counsels of both sides. Contentions/pleas of the parties, on various issues raised in the RP, Written Arguments, and Oral Arguments advanced during the hearing, are summed up below.
6.1.1 Counsel for the Complainant contended that the incident which occurred on 25.05.2005 was not the result of any deliberate or wilful act of the Petitioner and same be treated as an accident. Reliance has been placed by the counsel on the findings of the Hon’ble Supreme Court in Life Insurance Corporation V. Hira Lal ( 2011) 14 SCC 445 and order of this Commission in Maya Devi V. Life Insurance Corporation of India ( Manu/CF/75/2008) and Royal Sundaram Alliance Insurance Co. Ltd. Vs. Pawn Balram Mulchandani ( 2018) SCC Online Ncdrc 377.
6.1.2 It is further argued that once the Insurance Company has partially accepted the claim filed by the Complainant, Insurance Company is deemed to have accepted that an accident took place qua the Petitioner and therefore they are estopped from contending otherwise in proceedings for an enhanced sum of money.
6.1.3 Scheme of the policy cannot be unilaterally modified by the Insurer without the prior consent of the insured.
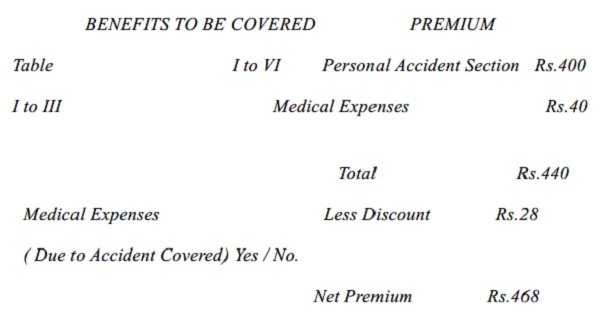
6.1.4 Complainant further argued that when Petitioner applied for insurance policy, he had premium of Rs.440/- which included Table I to Table III which covered benefit no. 1 to VI and benefit no. VI was in respect of Disability Bonus and from the year 2003, the Insurance Company unilaterally restricted the number of benefits offered to the Petitioner from Benefit Nos.1 to VI to Benefit No.1 to V. The Tables being offered to the Petitioner remained the same i.e. despite being offered Table No.1 to 3 the number of Benefits had gone down from VI to V and he came to know of the change when he applied for information under RTI Act.
6.1.5. The Petitioner was never informed about any such unilateral modifications made by the Insurance Company. Reliance was placed by the Complainant on the findings of the Hon’ble Supreme Court in Jacob Punnen Vs. United India Ins. Co. Ltd. ( 2022) 3 SCC 655.
6.1.6. The Petitioner also contended that relationship of Insurance Company and Insured is based on principle of Uberrima Fides i.e. of utmost good faith.
6.1.7. The Disability Bonus of 1% of CSI ( i.e. Rs.3,000/- ) per week subject to a maximum of Rs.5,000/- per week was payable to the Petitioner in terms of Benefit No.VI for the total number of weeks for which he was totally disabled from engaging in any employment.
6.1.8 In terms of Disability Bonus clause, the petitioner is entitled to sum of Rs.3,000/-per week for a period of 87 weeks i.e. Rs.3000 x 87 weeks = Rs.2,61,000/-.
6.1.9 The Petitioner is entitled for a total sum of Rs.3,30,000/- along with interest.
6.1.10 The Fora Below should have awarded interest from the submissions of claim form i.e. 25.08.2005. In this regard Complainant relied on the order of this Commission in case of Shriram General Insurance Co. Ltd. Vs. B. Sunitha ( 2019) SCC Online NCDRC 1619.
6.2.1 Counsel for the Respondents argued that there is an inordinate delay in filing the Revision Petition and no cogent reasons have been mentioned for condoning the delay.
6.2.2. The offer made by the Respondent to the Petitioner to settle the claim of Rs.1,50,000/- is in order and as per the terms and conditions of the policy of insurance.
6.2.3. The Respondent has already paid sum of Rs.2,11,125/- in satisfaction of Order dated 26.03.2018 of the State Commission and having accepted the amount, the Petitioner has forfeited his right to challenge the same.
6.2.4 The Petitioner has hidden the fact in the intimation letter that he was thrown from the roof top of his house by his wife and son due to some financial feud in the family and an FIR had been registered against his wife and son.
6.2.5 The Petitioner did not furnish the requisite documents and, therefore, the claim of the Petitioner was treated as no claim.
6.2.6 On the basis of document particularly the Medical Certificate issued by the Officer of Civil Surgeon cum Chief Medical Officer Vaishali, it was found to be case of 40% disablement of the foot and as per table 3 and terms and conditions of the Policy of Insurance a sum of Rs.1,50,000/- is payable.
6.2.7 Contract of Personal Insurance is an Annual Contract and is entered into a fresh every year on the expiry of earlier contract.
6.2.8. The fact that Respondent has remodelled the format of individual Personal Accident Policy as a whole for all the policy holders and that while remodelling the format due care had been taken to carry forward the benefit earned by the Policy Holder at the time of issuance of the policy for new period was fully in the knowledge of the Appellant.
6.2.9. The fact that policy is being issued on new format was also fully in the knowledge of the Appellant.
6.2.10 The claim has been duly considered and claim has been paid as per the terms and conditions of the policy.
6.2.11 Respondent has duly paid the benefit of permanent partial disablement.
7. The case of the Complainant is that under the Personal Accident Policy taken by him from the OP in 1993, which continued till 2005-06, on yearly renewal basis, he had opted for Table-III, which was the top table at that time, covering benefits no. 1 to 6, along with extension for medical expenses. Earlier policy number was 210106 but the same was subsequently changed to 210903. OP subsequently restructured the scheme and instead of 3 Tables in total, they divided the scheme in 4 different tables, wherein the benefits opted for and paid by the Complainant i.e. benefit nos. 1 to 6 have been put under newly formed Table-IV. It is the case of the complainant that despite charging him for all the benefits covered under the scheme, and Complainant having opted for the same, the OP continued to mention Table-III in the policy bonds instead of substituting it with the newly constituted Table-IV and the same was required to be corrected by the OP. Anyhow, even the policy of relevant year 2005-06 incorporates the said clause ( f) as being entitled to the Complainant under the policy.
8. The main dispute is relating to non payment of benefit under sub clause (f) ( corresponding to benefit no. 6 of the old policy) for which the Complainant has made following claim which had been disallowed by both District Forum and State Commission :
“1% of the CSI ( including CB) for 87 weeks ( the actual period the petitioner was totally disabled from engaging the employment) since 1 % of the CSI Rs.3009 x 87 = Rs.2,61,000/-.”
9. As is evident from the letter dated 23.01.2009 of the OP, following two claims totaling to Rs.1.50 lacs under clause / sub clause (e) and medical expenses, have been admitted by the OP :
“40% of the Capital Sum Insured ( CSI) ( including Cumulative Bonus ( CB) ) under sub-clause e (xii) of the policy ( corresponding to benefits No.5 read with entry No. xii in the old policy) since the petitioner has suffered 40% permanent partial disablement 40% of Rs.3,00,000/- = Rs. 1,20,000/-.
Medical expenses under extended medical benefit opted by the petitioner by paying 10% additional premium every year, amount to 10% of the CSI ( including CB) 10% of Rs.3,00,000/- = Rs.30000/-.”
10. While the District Forum allowed Rs.1.50 lacs without interest, State Commission allowed it with 9% interest. Hence, the issue for consideration is whether Complainant is entitled for claim of Rs.2.61 lacs under sub clause (f), corresponding to benefit no. 6 of the old policy, in addition to the claim of Rs.1.50 lacs allowed by the State Commission and District Forum.
11. The OP having admitted the claim of the Complainant to the extent of Rs.1.50 lacs as stated above, cannot at this stage again raise the issue whether the incident in question was accident or not. It is admitted by the OP that Complainant has taken the policy since 199293 continuously, that the contract of insurance is an annual contract, that as per terms and conditions of the contract, if any benefit has accrued to the policy holder at the end of the policy period, the same is carried forward as bonus in the next year policy contract, if entered to, that in the year 2002, the OP remodeled the format of individual personal accident policy as a whole for all the policy holders, that while remodeling the format, due care has been taken to carry forward the benefits earned by the policy holders at the time of issuance of the policy for the new period, that the OP issued policy for the year 2002-2003, 2004-2005, 2005-2006 on the new format, in these policies for respective years, the bonus earned by the Complainant was carried forward, that the policy is being issued on the new format was fully in the knowledge of the Complainant, he did not at any time during the period of three years raise any point on the issue which he is trying to raise now, that as per the terms and conditions of the policy at present or even earlier, the benefit of temporary disablement is an exclusion if the claim has been admitted for permanent or permanent partial disablement, that in this case the Complainant was entitled for benefit of permanent partial disablement, which has been duly considered and paid. However, we find that OP in their written submissions or oral arguments, have not given any specific response to the Complainant’s contention that he had opted for Table-III, which was the top table in the old policy, covering benefits 1 to 6, along with extension for medial expenses, but in the subsequent restructured policy, benefits under 1 to 6 have been put under the newly formed Table IV, but OP has continued to show him under Table – III under the restructured policy.
12. We have carefully gone through policy documents for the year 1996-97 to 2005-06. The State Commission has given no reasons for not accepting the claim of Rs.2.61 lacs, except stating that the ‘Appellant has not substantiated with documentary proof regarding claim of Rs.2.61 lacs’. A perusal of policy document for the year 1996-97 shows that under sub-clause ( f ), it contains the following entitlement :
“If such injury shall be sole and direct cause of temporary total disablement, then so long as the insured person shall be totally disabled from engaging in any employment or occupation of any description whatsoever a sum at the rate of one percent ( 1% ) of the capital sum insured stated in the schedule herein per week, but in any case not exceeding Rs.1500/- per week in all under all policies.”
13. Further, the Table of Benefits show that Table – III was the top Table and covered benefits 1 to 6. The relevant portion is reproduced below :
| Benefit No. | Description | Table | Benefits Covered |
| 1. | Death only… (100% if capital sum insured) | 1 | 1 |
| 2. | Loss of Two limbs of sight of two eyes or loss of one limb and loss of sight of one eye | ||
| 3. | Loss of one limb or loss of sight of one eye …. (50% of Capital sum insured) | ||
| 4. | Permanent total disablement from injuries other than named above…. (100% of Capita Sum Insured) | ||
| 5. | Permanent partial Disablement % page as shown below | II | 1 to 5 |
|
6. |
Temporary total disablement 1 % of Capital Sum Insured upto 104 weeks ( max. weekly benefits not exceeding Rs.1500/- |
III |
1 to 6 |
14. As per the policy, following were the exceptions :
1. Compensation under more than one of the foregoing sub-clauses in respect of the same period of disablement.
2. Any other payment to the same person after a claim under one of the sub-clauses (a), (b), (c) or (d) has been admitted and become payable.
3. Any payment in case of more than one claim under this Policy during any one period of insurance by which the maximum liability of the company in that period would exceed the sum payable under sub-clause (a) of the Policy
4. Payment of weekly compensation until the total amount shall have been ascertained and agreed.
5. Payment of compensation in respect of death, injury or disablement of insured—
(a) From intentional self-injury, suicide or attempted suicide
(b) Whilst under the influence of intoxicating liquor or drugs
(c) Whilst engaging in aviation or Ballooning, whilst mounting / dismounting from or traveling in any Balloon or aircraft other than as a passenger (fare paying or otherwise) in any duly Licensed Standard type of aircraft anywhere in the world (d) directly or indirectly caused by venereal disease or insanity ( e) arising or resulting from the insured committing any breach of law with criminal intent
6. Payment of compensation in respect of Death, Injury or disablement of the insured due to arising out of or directly or indirectly connected with or traceable to war, invasion, act of foreign enemy, Hostilities (whether war be declared or not) War, Rebellion, Revolution, Insurrection, Mutiny, Military or usurped Power, Seizure, Capture Arrests, Restraints and Detainment of all Kings, Princes and people of whatever nation, condition or quality so ever.
7. Payment of compensation in respect of Death of, or bodily injury or any disease or illness of the insured persons
a. Directly or indirectly caused by or contributed to by or arising from ionising radiation or contamination by radio activity substains from any nuclear fuel or from any nuclear waste from the combustion of nuclear fuel. For the purpose of this exception combustion shall include any self sustaining process of nuclear fission.
b. Directly or indirectly caused by or contributed to by or arising from nuclear weapon materials.
Provided also that the due observance and fulfillment of the terms and conditions of this Policy (which conditions and all endorsements hereon are to be read as part of this policy) shall so far as they relate to anything to be done or not to be done by the insured be a condition precedent to any liability of the company under this Policy No.
8. Pregnancy Exclusion Clause: The Insurance under this Policy shall not extend to cover death disablement resulting directly or indirectly from pregnancy or in consequence thereof.
15. The policy clearly states the Tables to be covered are Tables 1 to III and benefits to be covered are I to VI. Brief extracts of relevant portion is given below.
CAPITAL SUM INSURED
( a ) Sum Insured : Rs.2,00,000/- (Two lacs)
(b ) Commulative Bonus Earned Rs.30,000/- ( Thirty Thousand)
16. The document bears the seal of the OP and has not been denied by the OP. Keeping in view the above stated exceptions / clauses especially the one under Sl. No.1, we consider it necessary to reproduce all the entitlements:
“NOW THIS POLICY WITNESSETH that subject to the terms, conditions contained herein or endorsed or otherwise expressed hereon the Company will pay to the insured as hereinafter mentioned :
1. If at anytime during the currency of this policy the insured shall sustain any bodily injury resulting solely and directly from accident caused b external violent and visible means, then the company shall pay to the insured or his legal personal representative ( s ) as the case may be the sum or sums hereinafter set forth that is to say:
a) If such injury shall within twelve calendar month of its occurrence be the sole and direct cause to the death of the insured persons the Capital Sum insured stated in the Schedule hereto.
b) If such injury shall within 12 calendar months of its occurrence be the sole and direct cause of the total and irrecoverable loss of:
(i) Sight of both eyes, or the actual loss by physical separation of two entire hands or two entire feet, or one-entire hand and one entire foot or of such loss of sight of one eye and such loss of one entire foot, the capital sum insured stated in the Schedule hereto.
(ii) Use of hands or two feet, or of one hand one foot or such loss of sight of one eye and such loss of use of one hand or one foot, the capital sum insured stated in the Schedule herein.
(c) If such injury shall within twelve calendar months of its occurrence be the sole and direct cause of the total and irrecoverable loss of:
(i) The sight of one eye or of the actual loss by physical separation of one entire hand or one entire foot, fifty percent (50%) of the capital sum insured stated in the Schedule herein.
(ii) Total and irrecoverable loss of use of a hand or a foot without physical separation, fifty percent (50%) of the capital sum insured stated in the Schedule herein.
Note : For the purpose of clause ( b) and ( c ) above, physical separation of a hand or feet means separation of hands at or above the wrist and or of the foot at or above the ankle respectively.
(d) If such injury shall as a direct consequence thereof immediately permanently totally and absolutely, disable the insured person from engaging in any employment or occupation of any description whatsoever, then a lump sum equal to hundred percent (100%) of the Capital Sun Insured.
(e) If such injury shall within twelve calendar months of its occurrence be the sole and direct cause of the total and irrecoverable loss of use or the actual loss by physical separation of the following then the percentage of the Capital Sum Insured as indicated below shall be payable.
x x x x
(f) If such injury shall be sole and direct cause of temporary total disablement, then so long as the insured person shall be totally disabled from engaging in any employment or occupation of any description whatsoever a sum at the rate of one percent ( 1% ) of the capital sum insured stated in the schedule herein per week, but in any case not exceeding Rs.1500/- per week in all under all policies.
Provided the compensation payable under the foregoing sub-clauses (f) shall not be payable for more than 104 weeks in respect of any one injury calculated from the date of commencement of the disablement and in no case shall exceed the Capital sum insured.”
17. It is admitted by the Complainant that he has been paid / offered settlement of claim forRs.1.20 lacs under clause / sub clause ( e ) along with medical expenses under extended medical benefit opted. Now, the question arises, whether even under the old policy, before its restructuring in 2002, Complainant was entitled to benefits under multiple sub clause from (a ) to ( f) or only under one of the clause from ( a) to ( f) in view of exception no.1. The Exception no.1, as reproduced above, clearly states :
“Compensation under more than one of the foregoing sub-clauses in respect of the same period of disablement.”
Further the Exception no.2 states as follows:
“Any other payment to the same person after a claim under one of the sub- clauses (a), (b), ( c) or ( d) has been admitted and become payable.”
18. In view of the above stated exception clauses, we are of the view that Complainant is not entitled to benefits under multiple sub clauses. As his claim under clause / sub clause ( e) has been accepted, he cannot make additional claim under sub clause (f) due to exception clause. However, we are of the view that if the Complainant is to be given benefit of only one clause / sub clause, even though his case is covered under multiple clauses, he has a right to get his claim covered under the sub clause which gives him a higher benefit. Hence, although we find that he cannot claim benefit under both sub clauses ( e) and ( f), but has right to choose the sub clause which gives him the higher benefit. As clause / sub clause ( e) gives him a benefit of Rs.1.20 lacs but clause ( f) gives him a benefit of Rs.2.61 lacs, we are of the view that OP Insurance Company must give him the benefit under sub clause with higher monetary benefit. As was held by Hon’ble Supreme Court in Canara Bank Vs. United India Insurance Co. Ltd. & Ors. (2020) 3 SCC 455 that ‘Insurance Policy must be read holistically so as to give effect to reasonable expectations of all the parties including the insured and the beneficiaries- it must be interpreted in a commercially sensible manner-coverage clauses to be read broadly, and ambiguity, if any, to be resolved in favour of insured-exclusions to be read narrowly.”. Even if there is an ambiguity, the Consumer Protection Act being a beneficial legislation, it must be interpreted in favour of the consumer. Hence, we find that Complainant is entitled to claim of Rs.2.61 lacs under the policy in place of Rs.1.20 lacs, along with interest and with medical expenses under extended medical benefits (Rs.30,000/-). Hence, the State Commission’s / District Forum’s orders needs modification to this extent.
19. For the reasons stated hereinabove, and after giving a thoughtful consideration to the entire facts and circumstances of the case, various pleas raised by the learned Counsel for the Parties, the RP is partially allowed/disposed off with the following directions/reliefs: –
(i) OP ( Respondent herein) shall pay an amount of Rs.2.91 lacs (Rs.2.61 lacs under sub clause (f) plus Rs.30,000/- under extended medical benefit) to the Complainant (Petitioner herein), instead of Rs.1.50 lakh awarded by the State Commission / District Forum, along with interest @ 9% p.a. from 25.11.2005 ( six months from the date of incident) till the date of actual payment.
(ii) The Petitioner herein will be entitled to compensation of Rs.10,000/- as awarded by the State Commission.
(iii) The Petitioner herein will also be entitled to litigation cost of Rs.30,000/-, including the litigation cost of Rs.5000/- awarded by the State Commission.
(iv) All payments to be made by the OP within 2 months failing which it will carry interest @ 12%
20. The pending IAs in the case, if any, also stand disposed off.




