BRIHANMUMBAI MUNICIPAL CORPORATION
PUBLIC HEALTH DEPARTMENT
HO/35952-A dt. 06/01/2022
HOME ISOLATION GUIDELINES FOR PATIENTS & CAREGIVERS
Background
Over the past two years, it has been seen globally as well as in India that majority of cases of COVID-19 are either asymptomatic or have very mild symptoms. Such cases usually recover with minimal interventions and accordingly may be managed at home under proper medical guidance and monitoring.
BMC had issued the Home Isolation guidelines earlier, which is now revised for patients and care givers to guide them during home isolation. This guidelines are based on Government of India’s guidelines dated 5.1.2022.
The present guidelines are applicable to COVID-19 patients who have been clinically assessed and assigned as mild / asymptomatic cases of COVID-19.
Asymptomatic cases; mild cases of COVID-19
The asymptomatic cases are laboratory confirmed cases who are not experiencing any symptoms and have oxygen saturation at room air of more than 93%.
Clinically assigned mild cases are patients with upper respiratory tract symptoms with or without fever, without shortness of breath and having oxygen saturation at room air of more than 93%.
Patients eligible for Home Isolation
i. The patient should be clinically assigned as mild/ asymptomatic case by the treating Medical Officer.
ii. Such cases should have the requisite facility at their residence for self-isolation and for quarantining the family contacts. All the patients not having such facility will be shifted to designated CCC2.
iii. A caregiver (ideally someone who has completed his COVID-19 vaccination schedule) should be available to provide care on 24×7 basis A communication link between the caregiver and a Medical Officer of BMC is expected for the entire duration of home isolation.
iv. Elderly patients aged more than 60 years and those with co-morbid conditions such as Hypertension, Diabetes, Heart disease, Chronic lung / liver / kidney disease, Cerebrovascular disease etc. shall only be allowed home isolation after proper evaluation by the treating Medical Officer / Doctor.
v. Patients suffering from immune compromised status (HIV, Transplant recipients, Cancer therapy, etc.) are not recommended for home isolation and shall only be allowed home isolation after proper evaluation by the treating Medical Officer / Doctor
vi. While a patient is allowed home isolation, all other members in the family including other contacts shall follow the home quarantine guidelines
vii. Home Isolation shall not be applicable for pregnant women 2 weeks before Expected Date of Delivery (EDD).
Instructions for the patient
i. Patient must isolate himself from other household members, stay in the identified room and away from other people in home, especially elderly and those with co-morbid conditions like hypertension, cardiovascular disease, renal disease etc.
ii. The patient should stay in a well-ventilated room with cross ventilation and windows should be kept open to allow fresh air to come in.
iii. Patient should at all times use triple layer medical mask. They should discard mask after 8 hours of use or earlier if the mask becomes wet or is visibly soiled. In the event of Caregiver entering the room, both Caregiver and patient may preferably consider using N95 mask.
iv. Mask should be discarded after cutting them to pieces and putting in a paper bag for a minimum of 72 hours.
v. Patient must take rest and drink lot of fluids to maintain adequate hydration.
vi. Follow respiratory etiquette at all times.
vii. Undertake frequent hand washing with soap and water for at least 40 seconds or clean with alcohol-based sanitizer
viii. The patients shall not share personal items including utensils with other people in the household.
ix. Need to ensure cleaning of frequently touched surfaces in the room (tabletops, doorknobs, handles, etc.) with soap/detergent & water. The cleaning can be undertaken either by the patient or the caregiver duly following required precautions such as use of masks and gloves.
x. Self-monitoring of blood oxygen saturation with a pulse oximeter for the patient is advised.
xi. The patient shall self-monitor his/her health with daily temperature monitoring (as given below) and report promptly if any deterioration of symptom is noticed. The status shall be shared with the treating Medical Officer as well as surveillance teams/Control room.
Patients Self -health monitoring Chart
| Date and Time | Temperature | Heart rate (from pulse oximeter) | SpO2 % (from pulse oximeter) * | Feeling: (better / same / worse) | Breathing: (better / same / worse)** |
* For self-monitoring blood oxygen saturation with a pulse oximeter, place the index finger (after cleaning hands and removing nail polish, if any) in the pulse oximeter probe and take the highest steady reading after a few seconds.
**The patient may self-monitor breathing rate/respiratory rate in sitting position, breathe normally and count the number of breaths taken in 1 full minute.
Instructions for Care Giver
i. Mask:
- The caregiver should wear a triple layer medical mask. N95 mask may be considered when in the same room with the ill person.
- Front portion of the mask should not be touched or handled during use.
- If the mask gets wet or dirty with secretions, it must be changed immediately.
- Mask should be discarded after cutting them to pieces and putting in a paper bag for a minimum of 72 hours.
- Perform hand hygiene after disposal of the mask.
- He/she should avoid touching own face, nose or mouth.
ii. Hand hygiene:
- Hand hygiene must be ensured following contact with ill person or his immediate environment.
- Use soap and water for hand washing at least for 40 seconds. Alcohol-based hand rub can be used, if hands are not visibly soiled.
- After using soap and water, use of disposable paper towels to dry hands is desirable. If not available, use dedicated clean cloth towels and replace them when they become wet.
- Perform hand hygiene before and after removing gloves.
iii. Exposure to patient/patient’s environment:
- Avoid direct contact with body fluids (respiratory, oral secretions including saliva) of the patient. Use disposable gloves while handling the patient
- Avoid exposure to potentially contaminated items in his immediate environment (e.g. avoid sharing eating utensils, dishes, drinks, used towels or bed linen).
- Food must be provided to the patient in his room Utensils and dishes used by the patient should be cleaned with soap/detergent and water while wearing gloves. The utensils may be re-used after proper cleaning.
- Clean hands after taking off gloves or handling used items Use triple layer medical mask and disposable gloves while cleaning or handling surfaces, clothing or linen used by the patient.
- Perform hand hygiene before and after removing gloves.
iv. Biomedical Waste disposal:
- Effective and safe disposal of general wastes such as disposable items, used food packets. fruit peel offs, used water bottles, left-over food, disposable food plates etc. should be ensured. They should be collected in bags securely tied for handing over to waste collectors.
- Further, the used masks, gloves and tissues or swabs contaminated with blood / body fluids of COVID-19 patients, including used syringes, medicines, etc., should be treated as biomedical waste and disposed of accordingly by collecting the same in a yellow bag and handed over to waste collector separately so as to prevent further spread of infection within household and the community. Else they can be disposed of by putting them in appropriate deep burial pits which are deep enough to prevent access to rodents or dogs etc.
Treatment for patients with mild / asymptomatic disease in home isolation
i. Patients must be in communication with a treating Medical Officer / Doctor and promptly report in case of any deterioration.
ii. The patient must continue the medications for other co-morbidities/ illness after consulting the treating Medical Officer I Doctor.
iii. Patients to follow symptomatic management for fever, running nose and cough, as warranted.
iv. Patients may perform warm water gargles or take steam inhalation thrice a day.
v. If fever is not controlled with a maximum dose of Tab. Paracetamol 650 mg four times a day, consult the treating doctor
vi. Avoid misinformation on social media which are non-authentic or non-verified and hence avoid panic.
vii Do not rush for self-medication. blood investigation or radiological imaging like chest X ray or chest CT scan without consultation of your treating Medical Officer
viii Steroids are not indicated in mild disease and shall not be self-administered Overuse & inappropriate use of steroids may lead to additional complications
ix Treatment for every patient needs to be monitored individually as per the specific condition of the patient concerned and hence generic sharing of prescriptions shall be avoided
x. In case of falling oxygen saturation or shortness of breath, the person may require hospital admission and shall seek immediate consultation of their treating Medical Officer/surveillance team /Control room.
When to seek medical attention
Patient / Care giver will keep monitoring their health. Immediate medical attention must be sought if serious signs or symptoms develop. These could include-
i. High-grade fever (more than 100′ F for more than 3 days).
ii. Difficulty in breathing.
iii. Dip in oxygen saturation (SpO2 < 93% on room air at least 3 readings within 1 hour) or respiratory rate >24/ min
iv. Persistent pain/pressure in the chest.
v. Mental confusion or inability to arouse
vi. Severe fatigue and myalgia.
When to end Home Isolation
Patient under Home Isolation will stand discharged and end isolation after at least 7 days have passed from testing positive and no fever for 3 successive days and they shall continue wearing masks. There is no need for re-testing after the home isolation period is over
High risk contacts shall be home quarantined for 7 days. They shall be tested on 5th to 7th day or immediately if they turn symptomatic and further protocols shall be followed based on their test results. If negative end home quarantine.
Asymptomatic low risk contacts of infected individuals need not undergo COVID test.
Ward War Room list is attached herewith.
I S Chahal
Municipal Commissioner

BRIHANMUMBAI MUNICIPAL CORPORATION
PUBLIC HEALTH DEPARTMENT
HO / 35952 / C dt 06.01.2022
Roles and Responsibilities of Ward War Room
In view of exponential rise in cases in Mumbai, there will be many patients in home isolation who needs to be monitored by Ward War Room teams and bed allocation to needy patients. Hence, for smooth handling of positive cases and allotment of beds, following guidelines are issued for all MOsH, Ward War Rooms staff and Health Post . –
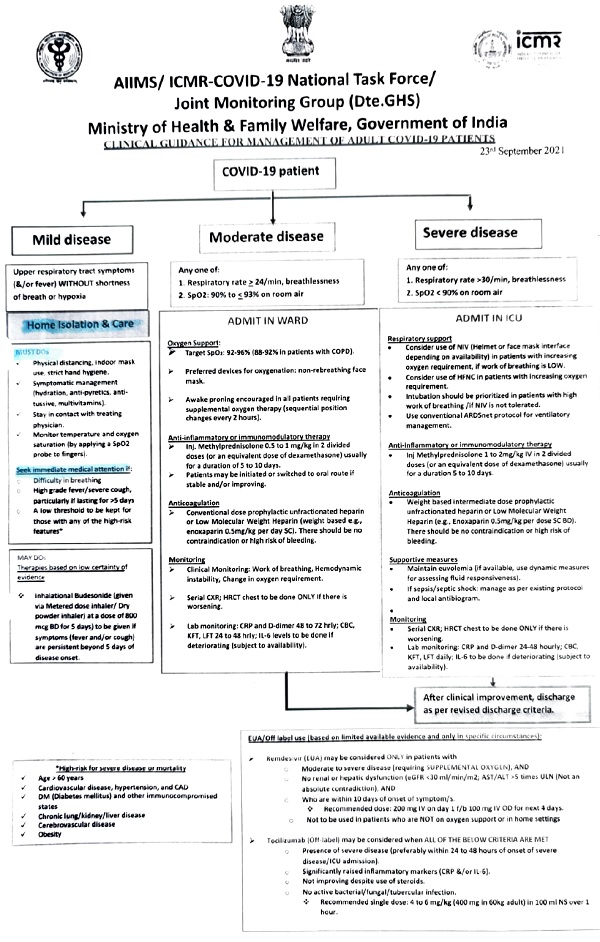
1. After receipt of COVID positive list, patient will be triaged by the medical officer/ doctor of ward war room team on the same day as asymptomatic, mild, moderate and severe.
- The asymptomatic cases are laboratory confirmed cases who are not experiencing any symptoms and have oxygen saturation at room air of more than 93%.
- Clinically assigned mild cases are patients with upper respiratory tract symptoms with or without fever, without shortness of breath and having oxygen saturation at room air of more than 93%.
- Mild cases without co-morbidity can be treated by War Room Medical Officer / Doctor symptomatically as per GOI protocols.
> antipyretics for fever
> antitussives and antihistaminics for cough and cold and
> supportive medicines like multi vitamin, Vitamin C, etc
- Doctor of Ward War Room should assess the patient based on:-
> The oxygen saturation
> Severity of symptoms
> Co-morbidities
> Vaccination status
- Bed shall be allocated to those patients who have SPO2 less than 93 or are co-morbid and symptomatic or breathless. In case of doubt, medical team can be sent home and treating physician can be consulted.
- For shifting such patients, ambulance shall be arranged. Coordination with concerned nodal officer of the hospital shall be made. Patient shall be allotted Non 02 bed, 02 bed or ICU/ Ventilator bed depending upon clinical condition. Patient should be given the choice of public and private hospitals.
- Any patient whose fever persists for more than 3 days or have other symptoms with co-morbidities, bed can be allocated to such patients for treatment and further investigations in consultation with treating physician.
- Asymptomatic & mild patients not having requisite facility for home isolation shall be shifted to CCC2
2. Assign home isolation for eligible patients as per the guidelines of home isolation.
3. The patient shall be informed to isolate himself / herself at home and self monitor daily. All the patients should be counseled as per the home isolation guidelines.
4. Emergency contact number of the Ward War Room to be given to the patient / relatives and explain about danger signs. Patient shall be assured that if needed beds will be made available, hence they need not panic.
5. Take the name and phone number of patients family doctor as well as connect to the doctor if required.
6. A register to be maintained at Ward War Room of daily calls made and daily calls received and attended by the Ward War Room.
7. Send the list of Home isolation patients assigned, to the Health Post for confirmation and follow up.
8. The patient will be marked in Quantela System as Home isolation on the same day War Room will notify MOH / Health Post staff of non-traceable patient.
9. All Ward war rooms will ensure that all the private hospitals will update the bed status—Oxygenated/ ICU/ Ventilators on the MCGM portal regularly for smooth bed allotment
Instructions for the Health Post Team
Health staff shall ensure follow-up of patients in Home Isolation / Home Care
> Health post team shall assess the suitability of the house for home isolation
> All the patients should be contacted on phone regularly by Health Post staff and ensure the patient’s condition is stable or if developed symptoms then advise accordingly. Contact the Ward War Room for shifting the patient if required.
> Ensure that home isolated patient monitors his / her health and takes treatment for COVID-19 from their family physician and continues co-morbidity treatment as it is regularly. He / She regularly informs their health status to the medical officer / physician / family doctor. Note down the name of the physician.
> Patients should be advised to keep the daily monitoring chart and ensure pulse oxymeter and other logistics like mask, sanitizer, thermometer, etc.
> Patient should restrict the movement within the house and should not attend functions or gatherings. Explain COVID appropriate behavior.
> The patients who do not have family physician then only on request Health Post AMO can advise treatment as per the protocol.
> All high risk contacts of patient should remain in home quarantine and be tested as per protocols. Explain the need for vaccination of all eligible in the house.
> Maintain a register of all the patients visited and followed up and of outcome.
I S. Chahal
Municipal Commissioner
Download Home Isolation Guidelines For Patients& Caregivers Background PDF




