Article compiles Guidelines on Clinical management of severe acute respiratory illness (SARI) in suspect/confirmed novel Coronavirus (nCoV) cases, Updated Travel advisory for travelers visiting China (to replace previous travel advisory), Guidance on Surveillance for human infection with 2019-nCoV, Guidelines for Infection Prevention and Control in Healthcare Facilities and Guidance for sample Collection, Packaging and Transportation for Novel Coronavirus.
Page Contents
- I. Guidelines on Clinical management of severe acute respiratory illness (SARI) in suspect/confirmed novel coronavirus (nCoV) cases
- II. Updated Travel advisory for travelers visiting China
- III. GUIDANCE DOCUMENT FOR POEs, STATES AND UTs FOR SURVEILLANCE OF 2019-nCoV
- IV. Guidelines for Infection Prevention and Control in Healthcare Facilities- Link
- V. Guidance for sample Collection, Packaging and Transportation for Novel Coronavirus
An infection with a novel coronavirus has been reported from China. As 25th January 2020, a total of 1287 cases and 41 deaths were reported in 29 provinces (districts and cities) of China. In addition, 28 cases have been confirmed outside Chinese mainland: 5 cases in Hong Kong, 2 cases in Macao, 3 cases in Taiwan, 4 cases in Thailand (2 cases cured), 2 cases in Japan (1 case cured), 2 cases in South Korea, 2 cases in the United States, 2 cases in Vietnam, 3 cases in Singapore, 1 case in Nepal and 2 cases in France.
Purpose and scope of document
This document is intended for clinicians taking care of hospitalised adult and paediatric patients with severe acute respiratory infection (SARI) when an nCoV infection is suspected. It is not meant to replace clinical judgment or specialist consultation but rather to strengthen clinical management of these patients and provide to up-to-date guidance. Best practices for SARI including IPC and optimized supportive care for severely ill patients are essential.
This document aims to provide clinicians with updated interim guidance on timely, effective, and safe supportive management of patients with nCoV and SARI, particularly those with critical illness. The recommendations in this document are derived from WHO publications.
A. Triage: Early recognition of patients with SARI associated with nCoV infection.
The purpose of triage is to recognize and sort all patients with SARI at first point of contact with health care system (such as the emergency department). Consider nCOV as a possible etiology of SARI under certain conditions (see Table 1). Triage patients and start emergency treatments based based on disease severity.
Table 1: Definitions of patients with SARI, suspected of nCoV*
| SARI | An ARI with history of fever or measured temperature ≥38 C° and cough; onset within the last ~10 days; and requiring hospitalization. However, the absence of fever does NOT exclude viral infection. |
| Surveillance case definitions for nCoV* | 1. Severe acute respiratory infection (SARI) in a person, with history of fever and cough requiring admission to hospital, with no other etiology that fully explains the clinical presentation1 (clinicians should also be alert to the possibility of atypical presentations in patients who are immunocompromised);
AND any of the following: a) A history of travel to Wuhan, Hubei Province China in the 14 days prior to symptom onset; or b) the disease occurs in a health care worker who has been working in an environment where patients with severe acute respiratory infections are being cared for, without regard to place of residence or history of travel; or c) the person develops an unusual or unexpected clinical course, especially sudden deterioration despite appropriate treatment, without regard to place of residence or history of travel, even if another etiology has been identified that fully explains the clinical presentation 2. A person with acute respiratory illness of any degree of severity who, within 14 days before onset of illness, had any of the following exposures: a) close physical contact2 with a confirmed case of nCoV infection, b) a healthcare facility in a country where hospital-associated nCoV infections have been reported; |
* see https://mohfw.gov.in/media/disease-alerts for latest case definition
1- Testing should be according to local guidance for management of community-acquired pneumonia. Examples of other etiologies include Streptococcus pneumoniae, Haemophilus influenza type B, Legionella pneumophila, other recognized primary bacterial pneumonias, influenza viruses, and respiratory syncytial virus.
2- Close contact is defined as:
- Health care associated exposure, including providing direct care for nCoV patients, working with health care workers infected with nCoV, visiting patients or staying in the same close environment of a nCoV patient
- Working together in close proximity or sharing the same classroom environment with a with nCoV patient
- Traveling together with nCoV patient in any kind of conveyance
- Living in the same household as a nCoV patient
The epidemiological link may have occurred within a 14-day period before or after the onset of illness in the case under consideration
Novel Coronavirus may present with mild, moderate, or severe illness; the latter includes severe pneumonia, ARDS, sepsis and septic shock. Early recognition of suspected patients allows for timely initiation of IPC (see Table 2). Early identification of those with severe manifestations (see Table 2) allows for immediate optimized supportive care treatments and safe, rapid admission (or referral) to intensive care unit according to institutional or national protocols. For those with mild illness, hospitalization may not be required unless there is concern for rapid deterioration. All patients discharged home should be instructed to return to hospital if they develop any worsening of illness.
Table 2: Clinical syndromes associated with nCoV infection
| Uncomplicated illness | Patients with uncomplicated upper respiratory tract viral infection, may have non-specific symptoms such as fever, cough, sore throat, nasal congestion, malaise, headache, muscle pain or malaise. The elderly and immunosuppressed may present with atypical symptoms. These patients do not have any signs of dehydration, sepsis or shortness of breath |
| Mild pneumonia | Patient with pneumonia and no signs of severe pneumonia.
Child with non-severe pneumonia has cough or difficulty breathing + fast breathing: fast breathing (in breaths/min): <2 months, ≥60; 2–11 months, ≥50; 1–5 years, ≥40 and no signs of severe pneumonia |
| Severe pneumonia | Adolescent or adult: fever or suspected respiratory infection, plus one of respiratory rate >30 breaths/min, severe respiratory distress, or SpO2 <90% on room air
Child with cough or difficulty in breathing, plus at least one of the following: central cyanosis or SpO2 <90%; severe respiratory distress (e.g. grunting, very severe chest indrawing); signs of pneumonia with a general danger sign: inability to breastfeed or drink, lethargy or unconsciousness, or convulsions. Other signs of pneumonia may be present: chest indrawing, fast breathing (in breaths/min): <2 months, ≥60; 2–11 months, ≥50; 1–5 years, ≥40. The diagnosis is clinical; chest imaging can exclude complications. |
| Acute Respiratory Distress Syndrome |
Onset: new or worsening respiratory symptoms within one week of known clinical insult.
Chest imaging (radiograph, CT scan, or lung ultrasound): bilateral opacities, not fully explained by effusions, lobar or lung collapse, or nodules. Origin of oedema: respiratory failure not fully explained by cardiac failure or fluid overload. Need objective assessment (e.g. echocardiography) to exclude hydrostatic cause of oedema if no risk factor present. Oxygenation (adults):
Oxygenation (children; note OI = Oxygenation Index and OSI = Oxygenation Index using SpO2)
|
| Sepsis | Adults: life-threatening organ dysfunction caused by a dysregulated host response to suspected or proven infection, with organ dysfunction. Signs of organ dysfunction include: altered mental status, difficult or fast breathing, low oxygen saturation, reduced urine output, fast heart rate, weak pulse, cold extremities or low blood pressure, skin mottling, or laboratory evidence of coagulopathy, thrombocytopenia, acidosis, high lactate or hyperbilirubinemia.
Children: suspected or proven infection and 22 SIRS criteria, of which one must be abnormal temperature or white blood cell count |
| Septic shock | Adults: persisting hypotension despite volume resuscitation, requiring vasopressors to maintain MAP 265 mmHg and serum lactate level >2 mmol/L
Children: any hypotension (SBP <5th centile or >2 SD below normal for age) or 2-3 of the following: altered mental state; tachycardia or bradycardia (HR <90 bpm or >160 bpm in infants and HR <70 bpm or >150 bpm in children); prolonged capillary refill (>2 sec) or warm vasodilation with bounding pulses; tachypnea; mottled skin or petechial or purpuric rash; increased lactate; oliguria; hyperthermia or hypothermia |
B. Immediate implementation of appropriate IPC measures
IPC is a critical and integral part of clinical management of patients and should be initiated at the point of entry of the patient to hospital (typically the Emergency Department). Standard precautions should always be routinely applied in all areas of health care facilities. Standard precautions include hand hygiene; use of PPE to avoid direct contact with patients’ blood, body fluids, secretions (including respiratory secretions) and non-intact skin. Standard precautions also include prevention of needle-stick or sharps injury; safe waste management; cleaning and disinfection of equipment; and cleaning of the environment.
Table 3: How to implement infection prevention and control measures for patients with suspected or confirmed nCoV infection
| At triage |
|
| Apply droplet precautions |
|
| Apply contact precautions |
|
| Apply airborne precautions when performing an aerosol generating procedure |
|
Abbreviations: ARI, acute respiratory infection; PPE, personal protective equipment
C. Early supportive therapy and monitoring
a. Give supplemental oxygen therapy immediately to patients with SARI and respiratory distress, hypoxaemia, or shock: Initiate oxygen therapy at 5 L/min and titrate flow rates to reach target SpO2 ?90% in non-pregnant adults and SpO2 ?92-95 % in pregnant patients. Children with emergency signs (obstructed or absent breathing, severe respiratory distress, central cyanosis, shock, coma or convulsions) should receive oxygen therapy during resuscitation to target SpO2 ?94%; otherwise, the target SpO2 is ?90%. All areas where patients with SARI are cared for should be equipped with pulse oximeters, functioning oxygen systems and disposable, single-use, oxygen-delivering interfaces (nasal cannula, simple face mask, and mask with reservoir bag). Use contact precautions when handling contaminated oxygen interfaces of patients with nCoV infection
b. Use conservative fluid management in patients with SARI when there is no evidence of shock: Patients with SARI should be treated cautiously with intravenous fluids, because aggressive fluid resuscitation may worsen oxygenation, especially in settings where there is limited availability of mechanical ventilation
c. Give empiric antimicrobials to treat all likely pathogens causing SARI. Give antimicrobials within one hour of initial patient assessment for patients with sepsis: Although the patient may be suspected to have nCoV, administer appropriate empiric antimicrobials within ONE hour of identification of sepsis. Empiric antibiotic treatment should be based on the clinical diagnosis (community-acquired pneumonia, health care-associated pneumonia [if infection was acquired in healthcare setting], or sepsis), local epidemiology and susceptibility data, and treatment guidelines. Empiric therapy includes a neuraminidase inhibitor for treatment of influenza when there is local circulation or other risk factors, including travel history or exposure to animal influenza viruses.18 Empiric therapy should be de-escalated on the basis of microbiology results and clinical judgment
d. Do not routinely give systemic corticosteroids for treatment of viral pneumonia or ARDS outside of clinical trials unless they are indicated for another reason: A systematic review of observational studies of corticosteroids administered to patients with SARS reported no survival benefit and possible harms (avascular necrosis, psychosis, diabetes, and delayed viral clearance). A systematic review of observational studies in influenza found a higher risk of mortality and secondary infections with corticosteroids; the evidence was judged as very low to low quality due to confounding by indication. A subsequent study that addressed this limitation by adjusting for time-varying confounders found no effect on mortality. Finally, a recent study of patients receiving corticosteroids for MERS used a similar statistical approach and found no effect of corticosteroids on mortality but delayed lower respiratory tract (LRT) clearance of MERS-CoV. Given lack of effectiveness and possible harm, routine corticosteroids should be avoided unless they are indicated for another reason. See section F for the use of corticosteroids in sepsis.
e. Closely monitor patients with SARI for signs of clinical deterioration, such as rapidly progressive respiratory failure and sepsis, and apply supportive care interventions immediately: Application of timely, effective, and safe supportive therapies is the cornerstone of therapy for patients that develop severe manifestations of nCoV
f. Understand the patient’s co-morbid condition(s) to tailor the management of critical illness and appreciate the prognosis: During intensive care management of SARI, determine which chronic therapies should be continued and which therapies should be stopped temporarily
g. Communicate early with patient and family: Communicate proactively with patients and families and provide support and prognostic information. Understand the patient’s values and preferences regarding life-sustaining interventions
D. Collection of specimens for laboratory diagnosis
Guidance on specimen collection, processing, transportation, including related biosafety procedures, is available on https://mohfw.gov.in/media/disease-alerts
Points to remember
- Collect blood cultures for bacteria that cause pneumonia and sepsis, ideally before antimicrobial therapy. DO NOT delay antimicrobial therapy to collect blood cultures
- Collect specimens from BOTH the upper respiratory tract (URT; nasopharyngeal and oropharyngeal) AND lower respiratory tract (LRT; expectorated sputum, endotracheal aspirate, or bronchoalveolar lavage) for nCoV testing by RT-PCR. Clinicians may elect to collect only LRT samples when these are readily available (for example, in mechanically ventilated patients)
- Use appropriate PPE for specimen collection (droplet and contact precautions for URT specimens; airborne precautions for LRT specimens). When collecting URT samples, use viral swabs (sterile Dacron or rayon, not cotton) and viral transport media. Do not sample the nostrils or tonsils. In a patient with suspected novel coronavirus, especially with pneumonia or severe illness, a single URT sample does not exclude the diagnosis, and additional URT and LRT samples are recommended. LRT (vs. URT) samples are more likely to be positive and for a longer period. Clinicians may elect to collect only LRT samples when these are readily available (for example, in mechanically ventilated patients). Sputum induction should be avoided due to increased risk of increasing aerosol transmission.
Dual infections with other respiratory viral infections have been found in SARS and MERS cases. At this stage we need detailed microbiologic studies in all suspected cases. Both URT and LRT specimens can tested for other respiratory viruses, such as influenza A and B (including zoonotic influenza A), respiratory syncytial virus, parainfluenza viruses, rhinoviruses, adenoviruses, enteroviruses (e.g. EVD68), human metapneumovirus, and endemic human coronaviruses (i.e. HKU1, OC43, NL63, and 229E). LRT specimens can also be tested for bacterial pathogens, including Legionella pneumophila
In hospitalized patients with confirmed nCoV infection, repeat URT and LRT samples should be collected to demonstrate viral clearance. The frequency of specimen collection will depend on local circumstances but should be at least every 2 to 4 days until there are two consecutive negative results (both URT and LRT samples if both are collected) in a clinically recovered patient at least 24 hours apart. If local infection control practice requires two negative results before removal of droplet precautions, specimens may be collected as often as daily
E. Management of hypoxemic respiratory failure and ARDS
Recognize severe hypoxemic respiratory failure when a patient with respiratory distress is failing standard oxygen therapy. Patients may continue to have increased work of breathing or hypoxemia even when oxygen is delivered via a face mask with reservoir bag (flow rates of 10-15 L/min, which is typically the minimum flow required to maintain bag inflation; FiO2 0.60-0.95). Hypoxemic respiratory failure in ARDS commonly results from intrapulmonary ventilation-perfusion mismatch or shunt and usually requires mechanical ventilation
High-flow nasal oxygen (HFNO) or non-invasive ventilation (NIV) should only be used in selected patients with hypoxemic respiratory failure. The risk of treatment failure is high in patients with MERS treated with NIV, and patients treated with either HFNO or NIV should be closely monitored for clinical deterioration. HFNO systems can deliver 60 L/min of gas flow and FiO2 up to 1.0; paediatric circuits generally only handle up to 15 L/min, and many children will require an adult circuit to deliver adequate flow. Compared to standard oxygen therapy, HFNO reduces the need for intubation. Patients with hypercapnia (exacerbation of obstructive lung disease, cardiogenic pulmonary oedema), hemodynamic instability, multi-organ failure, or abnormal mental status should generally not receive HFNO, although emerging data suggest that HFNO may be safe in patients with mild-moderate and non-worsening hypercapnia.25 Patients receiving HFNO should be in a monitored setting and cared for by experienced personnel capable of endotracheal intubation in case the patient acutely deteriorates or does not improve after a short trial (about 1 hr). Evidence-based guidelines on HFNO do not exist, and reports on HFNO in MERS patients are limited.
NIV guidelines make no recommendation on use in hypoxemic respiratory failure (apart from cardiogenic pulmonary oedema and post-operative respiratory failure) or pandemic viral illness (referring to studies of SARS and pandemic influenza). Risks include delayed intubation, large tidal volumes, and injurious transpulmonary pressures. Limited data suggest a high failure rate when MERS patients receive NIV. Patients receiving a trial of NIV should be in a monitored setting and cared for by experienced personnel capable of endotracheal intubation in case the patient acutely deteriorates or does not improve after a short trial (about 1 hr). Patients with hemodynamic instability, multiorgan failure, or abnormal mental status should not receive NIV.
Recent publications suggest that newer HFNO and NIV systems with good interface fitting do not create widespread dispersion of exhaled air and therefore should be associated with low risk of airborne transmission.
Endotracheal intubation should be performed by a trained and experienced provider using airborne precautions. Patients with ARDS, especially young children or those who are obese or pregnant, may desaturate quickly during intubation. Pre-oxygenate with 100% FiO2 for 5 minutes, via a face mask with reservoir bag, bag-valve mask, HFNO, or NIV. Rapid sequence intubation is appropriate after an airway assessment that identifies no signs of difficult intubation.
Implement mechanical ventilation using lower tidal volumes (4–8 ml/kg predicted body weight, PBW) and lower inspiratory pressures (plateau pressure <30 cmH2O). This is a strong recommendation from a clinical guideline for patients with ARDS, and is suggested for patients with sepsis-induced respiratory failure who do not meet ARDS criteria. The initial tidal volume is 6 ml/kg PBW; tidal volume up to 8 ml/kg PBW is allowed if undesirable side effects occur (e.g. dyssynchrony, pH <7.15). Hypercapnia is permitted if meeting the pH goal of 7.30-7.45. Ventilator protocols are available. The use of deep sedation may be required to control respiratory drive and achieve tidal volume targets. Although high driving pressure (plateau pressure−PEEP) may more accurately predict increased mortality in ARDS compared to high tidal volume or plateau pressure, RCTs of ventilation strategies that target driving pressure are not currently available.
In patients with severe ARDS, prone ventilation for >12 hours per day is recommended. Application of prone ventilation is strongly recommended for adult and paediatric patients with severe ARDS but requires sufficient human resources and expertise to be performed safely.
Use a conservative fluid management strategy for ARDS patients without tissue hypoperfusion.
In patients with moderate or severe ARDS, higher PEEP instead of lower PEEP is suggested. PEEP titration requires consideration of benefits (reducing atelectrauma and improving alveolar recruitment) vs. risks (end-inspiratory overdistension leading to lung injury and higher pulmonary vascular resistance). Tables are available to guide PEEP titration based on the FiO2 required to maintain SpO2. A related intervention of recruitment manoeuvres (RMs) is delivered as episodic periods of high continuous positive airway pressure [30–40 cm H2O], progressive incremental increases in PEEP with constant driving pressure, or high driving pressure; considerations of benefits vs. risks are similar. Higher PEEP and RMs were both conditionally recommended in a clinical practice guideline. For PEEP, the guideline considered an individual patient data meta-analysis of 3 RCTs. However, a subsequent RCT of high PEEP and prolonged high-pressure RMs showed harm, suggesting that the protocol in this RCT should be avoided. Monitoring of patients to identify those who respond to the initial application of higher PEEP or a different RM protocol, and stopping these interventions in non-responders, is suggested.
In patients with moderate-severe ARDS (PaO2/FiO2 <150), neuromuscular blockade by continuous infusion should not be routinely used. One trial found that this strategy improved survival in patients with severe ARDS (PaO2/FiO2 <150) without causing significant weakness, but results of a recent larger trial found that use of neuromuscular blockage with high PEEP strategy was not associated with survival when compared to a light sedation strategy without neuromuscular blockade. Continuous neuromuscular blockade may still be considered in patients with ARDS in certain situations: ventilator dyssnchony despite sedation, such that tidal volume limitation cannot be reliably achieved; or refractory hypoxemia or hypercapnia.
In settings with access to expertise in extracorporeal life support (ECLS), consider referral of patients with refractory hypoxemia despite lung protective ventilation. A recent guideline made no recommendation about ECLS in patients with ARDS. Since then, an RCT of ECLS for patients with ARDS was stopped early and found no statistically significant difference in the primary outcome of 60-day mortality between ECLS and standard medical management (including prone positioning and neuromuscular blockade). However, ECLS was associated with a reduced risk of the composite outcome of mortality and crossover to ECLS, and a post hoc Bayesian analysis of this RCT showed that ECLS is very likely to reduce mortality across a range of prior assumptions. In patients with MERS-CoV infection, ECLS vs. conventional treatment was associated with reduced mortality in a cohort study. ECLS should only be offered in expert centres with a sufficient case volume to maintain expertise and that can apply the IPC measures required for nCoV patients
Avoid disconnecting the patient from the ventilator, which results in loss of PEEP and atelectasis. Use in-line catheters for airway suctioning and clamp endotracheal tube when disconnection is required (for example, transfer to a transport ventilator)
F. Management of septic shock
Recognize septic shock in adults when infection is suspected or confirmed AND vasopressors are needed to maintain mean arterial pressure (MAP) ≥65 mmHg AND lactate is ≥2 mmol/L, in absence of hypovolemia. Recognize septic shock in children with any hypotension (systolic blood pressure [SBP] <5th centile or >2 SD below normal for age) or 2-3 of the following: altered mental state; tachycardia or bradycardia (HR <90 bpm or >160 bpm in infants and HR <70 bpm or >150 bpm in children); prolonged capillary refill (>2 sec) or warm vasodilation with bounding pulses; tachypnea; mottled skin or petechial or purpuric rash; increased lactate; oliguria; hyperthermia or hypothermia.
In the absence of a lactate measurement, use MAP and clinical signs of perfusion to define shock. Standard care includes early recognition and the following treatments within 1 hour of recognition: antimicrobial therapy and fluid loading and vasopressors for hypotension. The use of central venous and arterial catheters should be based on resource availability and individual patient needs. Detailed guidelines are available for the management of septic shock in adults and children.
In resuscitation from septic shock in adults, give at least 30 ml/kg of isotonic crystalloid in adults in the first 3 hours. In resuscitation from septic shock in children in well-resourced settings, give 20 ml/kg as a rapid bolus and up to 40-60 ml/kg in the first 1 hr.
Do not use hypotonic crystalloids, starches, or gelatins for resuscitation.
Fluid resuscitation may lead to volume overload, including respiratory failure. If there is no response to fluid loading and signs of volume overload appear (for example, jugular venous distension, crackles on lung auscultation, pulmonary oedema on imaging, or hepatomegaly in children), then reduce or discontinue fluid administration. This step is particularly important where mechanical ventilation is not available. Alternate fluid regimens are suggested when caring for children in resource-limited settings.
Crystalloids include normal saline and Ringer’s lactate. Determine need for additional fluid boluses (250-1000 ml in adults or 10-20 ml/kg in children) based on clinical response and improvement of perfusion targets. Perfusion targets include MAP (>65 mmHg or age-appropriate targets in children), urine output (>0.5 ml/kg/hr in adults, 1 ml/kg/hr in children), and improvement of skin mottling, capillary refill, level of consciousness, and lactate. Consider dynamic indices of volume responsiveness to guide volume administration beyond initial resuscitation based on local resources and experience. These indices include passive leg raises, fluid challenges with serial stroke volume measurements, or variations in systolic pressure, pulse pressure, inferior vena cava size, or stroke volume in response to changes in intrathoracic pressure during mechanical ventilation.
Starches are associated with an increased risk of death and acute kidney injury vs. crystalloids. The effects of gelatins are less clear, but they are more expensive than cyrstalloids. Hypotonic (vs. isotonic) solutions are less effective at increasing intravascular volume. Surviving Sepsis also suggests albumin for resuscitation when patients require substantial amounts of crystalloids, but this conditional recommendation is based on low-quality evidence.
Administer vasopressors when shock persists during or after fluid resuscitation. The initial blood pressure target is MAP ≥65 mmHg in adults and age-appropriate targets in children.
If central venous catheters are not available, vasopressors can be given through a peripheral IV, but use a large vein and closely monitor for signs of extravasation and local tissue necrosis. If extravasation occurs, stop infusion. Vasopressors can also be administered through intraosseous needles.
If signs of poor perfusion and cardiac dysfunction persist despite achieving MAP target with fluids and vasopressors, consider an inotrope such as dobutamine
Vasopressors (i.e. norepinephrine, epinephrine, vasopressin, and dopamine) are most safely given through a central venous catheter at a strictly controlled rate, but it is also possible to safely administer them via peripheral vein and intraosseous needle. Monitor blood pressure frequently and titrate the vasopressor to the minimum dose necessary to maintain perfusion and prevent side effects. Norepinephrine is considered first-line in adult patients; epinephrine or vasopressin can be added to achieve the MAP target. Because of the risk of tachyarrhythmia, reserve dopamine for selected patients with low risk of tachyarrhythmia or those with bradycardia. In children with cold shock (more common), epinephrine is considered first-line, while norepinephrine is used in patients with warm shock (less common).
G. Prevention of complications
Implement the following interventions (Table 4) to prevent complications associated with critical illness. These interventions are based on Surviving Sepsis or other guidelines, and are generally limited to feasible recommendations based on high quality evidence.
Table 4: Prevention of complications
| Anticipated Outcome | Interventions |
| Reduce days of invasive mechanical ventilation |
|
| Reduce incidence of ventilator associated pneumonia |
|
| Reduce incidence of venous thromboembolism |
|
| Reduce incidence of catheter related bloodstream infection |
|
| Reduce incidence of pressure ulcers |
|
| Reduce incidence of stress ulcers and gastrointestinal bleeding |
|
| Reduce incidence of ICU-related weakness |
|
H. Specific anti-Novel-CoV treatments and clinical research
There is no current evidence from RCTs to recommend any specific anti-nCoV treatment for patients with suspected or confirmed nCoV. Unlicensed treatments should be administered only in the context of ethically-approved clinical trials or the Monitored Emergency Use of Unregistered Interventions Framework (MEURI), with strict monitoring.
Clinical characterization protocols are available, including the SPRINT-SARI https://isaric.tghn.org/sprint-sari/ and WHOISARIC forms available at
https://isaric.tghn.org/protocols/severe-acute-respiratory-infection-data-tools/.
I. Special considerations for pregnant patients
Pregnant women with suspected or confirmed nCoV should be treated with supportive therapies as described above, taking into account the physiologic adaptations of pregnancy.
The use of investigational therapeutic agents outside of a research study should be guided by individual risk-benefit analysis based on potential benefit for mother and safety to fetus, with consultation from an obstetric specialist and ethics committee.
Emergency delivery and pregnancy termination decisions are challenging and based on many factors: gestational age, maternal condition, and fetal stability. Consultations with obstetric, neonatal, and intensive care specialists (depending on the condition of the mother) are essential.
Note: These guidelines are preliminary in nature and will be updated as soon as more information on clinical profile and treatment are available.
II. Updated Travel advisory for travelers visiting China
Novel coronavirus outbreak in China
Travel advisory to travelers visiting China
An infection with a novel coronavirus has been reported from China. As 25th January 2020, a total of 1287 cases and 41 deaths were reported in 29 provinces (districts and cities) of China. In addition, 28 cases have been confirmed outside Chinese mainland: 5 cases in Hong Kong, 2 cases in Macao, 3 cases in Taiwan, 4 cases in Thailand (2 cases cured), 2 cases in Japan (1 case cured), 2 cases in South Korea, 2 cases in the United States, 2 cases in Vietnam, 3 cases in Singapore, 1 case in Nepal and 2 cases in France.
The clinical signs and symptoms are mainly fever with a few patients having difficulty in breathing.
Mode of transmission is unclear but available evidence points to human-to-human transmission occurring between close contacts through respiratory route.
In view of the spurt of cases being reported from China and travel related cases appearing in many countries, the travelers to China are advised the following:
- Those planning a visit to China
- All non-essential travel to China to be avoided.
- Travelers to China should follow simple public health measures at all times as under:
- Observe good personal hygiene.
- Practice frequent hand washing with soap.
- Follow respiratory etiquettes – cover your mouth when coughing or sneezing.
- Avoid close contact with people who are unwell or showing symptoms of illness, such as cough, runny nose etc.
- Avoid contact with live animals and consumption of raw/undercooked meats.
- Avoid travel to farms, live animal markets or where animals are slaughtered.
- Wear a mask if you have respiratory symptoms such as cough or runny nose.
- All travelers to China to monitor their health closely
- During your stay in China, if you feel sick and have fever and cough:
- Cover your mouth while coughing or sneezing.
- Don’t plan any further travel, if sick.
- Seek medical attention promptly.
- Report to Indian Embassy in China ( +8618612083629 and +8618612083617)
- If you feel sick on flight, while traveling back to India:
- Inform the airlines crew about illness.
- Seek mask and the self-reporting format from the airline crew.
- Avoid close contact with family members or fellow travelers.
- Follow the directions of airline crew while disembarking.
- Immediately report facts to the Airport Health Office/Immigration Office and Helpline
number (011-23978046) also. - Follow the direction of the airport health officer or as issued by the helpline.
- If you feel sick within a span of one month after return from China:
- Immediately call the Helpline number (011-23978046) and follow the direction issued.
- Maintain effective self-isolation at home and with others.
- Observe good personal hygiene.
- Practice frequent hand washing with soap.
- Follow respiratory etiquettes – cover your mouth when coughing or sneezing.
- Report the illness to the nearest health facility and also inform the treating doctor regarding your travel history.
III. GUIDANCE DOCUMENT FOR POEs, STATES AND UTs FOR SURVEILLANCE OF 2019-nCoV
Situation Update (as on 25 January, 2020)
The Ministry of Health and Family Welfare (MoHFW), GoI is closely monitoring the outbreak of respiratory illness caused by a novel (new) coronavirus (termed “2019-nCoV”) that was first detected in Wuhan City, Hubei Province, China and which continues to expand.
As 25th January 2020, a total of 1287 cases and 41 deaths were reported in 29 provinces (districts and cities) of China. In addition, 28 cases have been confirmed outside Chinese mainland: 5 cases in Hong Kong, 2 cases in Macao, 3 cases in Taiwan, 4 cases in Thailand (2 cases cured), 2 cases in Japan (1 case cured), 2 cases in South Korea, 2 cases in the United States, 2 cases in Vietnam, 3 cases in Singapore, 1 case in Nepal and 2 cases in France.
Coronaviruses are a large family of viruses, some causing illness in people and others that circulate among animals, including camels, cats and bats. Rarely, animal coronaviruses can evolve and infect people and then spread between people such as has been seen with MERS and SARS.
Initially, many cases reported in the outbreak in Wuhan, China had some link to a large seafood and animal market, suggesting animal-to-person spread. However, with increased number of cases being reported without any history of exposure to animal markets, suggests person-to-person transmission might be occurring. At this time, it’s unclear whether the human to human transmission is sustainable or not.
Limited information is available to characterize the spectrum of clinical illness, however yet modes of transmission, incubation period and period of communicability is unknown. No vaccine or specific treatment for 2019-nCoV infection is available; supportive care is recommended.
This is a rapidly evolving situation and information will be updated as it becomes available. These guidelines have been developed based on what currently is known about the disease and guidance from WHO. These are subject to change as additional information becomes available at a short notice.
Risk assessment: WHO assesses the risk of this event to be very high in China, high at the regional level and moderate at the global level.
Currently, WHO has not declared the situation as PHEIC.
Response from MoHFW(GoI):
- MoHFW is closely monitoring this situation in collaboration with WHO.
- MoHFW has initiated inflight announcements with regard to nCoV and entry screening for travellers from 2019-nCoV affected countries (China) at designated airports
- Mechanism for in country surveillance and contact tracing has been put in place through Integrated Disease Surveillance Programme (IDSP), NCDC.
- Advisories for travellers visiting China and arriving from China have been issued.
- Public health preparedness including diagnostics, hospital preparedness, IPC, response, logistics is being constantly reviewed.
- Risk Communication has been initiated and signages have been displayed at PoEs.
Scope of the guidance: It is mainly targeted towards health personnel involved in entry screening at Points of Entries (designated Airports) and in community surveillance through the mechanism of IDSP.
Objectives of the guidance:
- To establish system for screening of travellers from 2019 nCoV affected countries (China) at Points of Entries:
- In flight announcement and filling of Self declaration form in the flight (Annexure 1)
- Suspect case of 2019nCoV based on WHO case definition (identified during screening at APHO) will be referred to designated Hospital and information shared with CSU IDSP/NCDC immediately (Annexure 6).
- Close contacts of the suspect case (co passengers seated in the same row, 3 rows in front and 3 rows behind along with some of the cabin crew) – Information be shared as per interim guidelines (page no. 5) in the format (Annexure 2 )
- List of passengers who have history of close contact (as per self declaration form)will be shared to IH Division and State/District for in-country surveillance by IDSP on daily basis.
- To establish In country/ community surveillance through the Integrated Disease Surveillance Programme network(IDSP)
- SSU/DSU will receive line list / emails of Passengers under observation, coming from 2019-nCoV affected countries* from APHO, Office of Emergency Medical Relief, MEA or CSU and information collected in Format A & B. (Annexure 3 & 4 )
- Health Status of these passengers to be shared with CSU in Format C (Annexure 5) as per SoPs (Page no. 3 ).
- Passengers who have history of close contact will be followed by IDSP officials on daily basis.
- Close contacts of the suspect case – Information be shared as per interim guidelines in the format (Annexure 2)
PROTOCOL FOR SENDING DAILY HEALTH STATUS OF PASSENGERS UNDER OBSERVATION SOPs for SSOs
1) SSU will receive line list / emails of Passengers under observation, coming from 2019-nCoV affected countries* from APHO, Office of Emergency Medical Relief, MEA or CSU.
2) SSU will share the line list / mails with DSUs immediately and Ensure immediate tracing of Passengers under observation by DSUs.
3) Information regarding any passenger who travels to another State will be immediately notified to the concerned State Health authority and comment shared in Format C.
4) SSU will receive complete investigation details in enclosed Format A from DSU as soon as possible on the same day.
5) SSU will ensure daily follow up of Passengers under observation for 28 days starting from date of last exposure/arrival.
6) SSU to compile the line list of all Passengers under observation daily, updating daily health status of Travelers / Suspects in enclosed Format B and share daily report of health status of Passengers under observation with CSU / EMR daily (Format C).
7) If any passenger is not traceable initially or during any duration while being followed up should be immediately notified to CSU.
All SSUs will keep themselves updated by routinely checking WHO and NCDC website on 2019-nCoV. Any guidelines shared by MoHFW on 2019-nCoV will be disseminated to concerned State/District authorities.
SOPs for DSU
1) Receive line list/ email of Passengers under observation from SSU/CSU/APHO.
2) Immediately trace the Passengers under observation and begin investigation and fill the enclosed format A. On first visit, passenger is to be provided a mask to be put on immediately in case symptoms such as fever and cough develop.
3) Passenger will be provided following advice during first visit by Health care provider:
a. You will also receive daily calls/visit from health department to ask your health status for the day, kindly cooperate with them.
b. You are requested to self-monitor for development of symptoms suggestive of 2019-nCoV i.e. Fever and Cough for 28 days from the date of arrival from 2019-nCoV affected countries*.
c. In case you initiation of symptoms (fever and cough), put on the mask immediately, restrict your outdoor movement and contact 24 hours helpline number 01123978046. The Call operator will tell you whom to contact further. In the meanwhile, keep yourself isolated in your house/room.
4) DSU has to ensure daily follow up of Passengers under observation for 28 days starting from date of possible exposure/arrival. Passengers will also be counseled for self-reporting of illness suggestive of 2019-nCoV.
5) Information regarding any passenger who travels to another District will be immediately notified to the concerned District Health authority and SSU.
6) In case, Passengers under observation develop symptoms suggestive of ARI/ILI, S/he has to be shifted to identified health facility with isolation unit (as transmission pattern of the virus is still unclear).Laboratory guidelines will be shared soon.
7) Daily follow up of Passengers under observation to be continued for 28 days starting from the date of last exposure/departure.
8) If any passenger is not traceable initially or during any duration while being followed up should be immediately notified to SSU/CSU.
9) Daily health status to be shared with SSU every day by 12:00 PM.
*Currently China only.
Advisory:
1. Format C to be sent positively every day to idsp-npo@nic.inby 12:00 pm including ‘Nil’ report.
2. The passenger has to be observed from 28 days from the day of possible exposure/arrival to India.
3. In case passenger develop any symptom, s/he will be requested to wear amask. Health care provider will arrange for the transfer of such patient from home to isolation facility. During the procedure, standard infection control practice for eg. wearing mask and hand washing should be performed by Health care providers.
Interim Guidelines for community based Tracing and Management of Contacts for 2019- nCoV Case
Contact tracing: the process
Contact tracing is the process of identifying, assessing, and managing people who have been exposed to a disease to prevent onward transmission. People who may have been exposed to 2019-nCoV are to be followed for 28 days from the date of the probable last exposure/arrival from 2019-nCoV affected countries.
Any person who has had contact with a patient under investigation/treatment for suspected, probable or confirmed case of 2019-nCoV (refer WHO case definition) should be carefully monitored for the appearance of symptoms of 2019-nCoV.
Contact is defined as:
Anyone who provided care for the suspect or confirmed case, including a health care worker or family member, or who had other similarly close physical contact;
Anyone who stayed at the same place (e.g. lived with, visited) while the suspect or confirmed case was symptomatic.
Note: This should include health workers (including those involved in cleaning, waste management, laboratory technicians, healthcare workers, etc.)
If symptoms of 2019-nCoV appear within the first 28 days following the contact, the individual should be considered a probable case and reported through IDSP network to NCDC.
Community based Contact Tracing Implementation Guidelines
1. As soon as the single event (identification of suspect or confirmed case) is detected, contact tracing must be aggressively implemented (preferably to be completed within 48 hours).
2. The contact tracing shall preferably be done by visiting the local residence of the contact(s) by a Health Personnel. Other methods of communication like telephone may be used in certain circumstances or for follow-up.
3. On meeting the ‘contact person’ the visiting Health Personnel should introduce him (her)-self, explain the purpose of contact tracing and should collect data in the prescribed format (Annex).
4. Contact tracing must include identification of extended social networks and travel history of cases during the 28 days after onset of illness.
5. Contacts of confirmed cases should be traced and monitored for at least 28 days after the last exposure to the case patient for evidence of 2019-nCoV symptoms as per case definition.
6. Information about contacts can be obtained from: a. Patient, his/her family members, persons at patient’s workplace or school associates, or b. others with knowledge about the patient’s recent activities and travels.
7. Case wise Line-listing (Performa enclosed at Annex) of all exposed contacts shall be maintained with the following information: a. demographic information, b. date of last exposure or date of contact with the case patient, c. date of onset of fever orother symptoms developed, if any.
Advisory for Symptomatic contacts:
Refer persons with fever and cough and history of contact with a confirmed case within last 28 days for:
1. Isolation for strict infection control
2. Collection and transportation of sample for laboratory testing at designated lab.
3. Appropriate medical care for management of patient.
Depending on the severity of illness, acceptability, and availability of hospital beds, ill contacts may be isolated at a health-care facility or at home while awaiting test-results. However, once confirmed by laboratory, such cases must be managed in a designated health facility.
Advisory for Asymptomatic Contacts:
- Remain at home (home quarantine) for at least 28 days after the last exposure with the case.
- Initiate self-health monitoring for the development of fever or cough within 28 days after the last exposure to the case patient and maintain a list of contacts on daily basis.
- If above described symptoms develop, person must put on the mask, self-isolate him in the home and inform the identified Local Health Official/District CMO/DSO by telephone and further management must be done at a designated health facility.
- Active monitoring (e.g. daily visits or telephone calls) for 28 days after the last exposure shall be done by the identified Local Health Officials.
Health and safety precautions for the contact tracing official:
- Maintain a distance of at least 2 meter (as advised by WHO*) from the contact.
- Personal protective equipment (PPE) is not needed for Contact Follow-up Teams and should not be worn. However, masks should be worn by the contact tracing team.
- Maintain standard infection prevention and control measures and hand washing should be performed.
Download Full Text All Guidance document – 2019 Annexure
IV. Guidelines for Infection Prevention and Control in Healthcare Facilities- Link
Title: Specimen Collection, Packaging and Transport Guidelines for 2019 Novel Coronavirus(2019-nCoV)
Scope: To be used by the Government health authorities/ hospitals/ clinicians/ laboratories planning to collect appropriat clinical samples as indicated for diagnosis of 2019-nCoV.
Purpose: This document describes the information for collection, packaging and transport of clinical specimens to Influenza group at ICMR-National Institute of Virology (NIV), Pune, Maharashtra for diagnosis of 2019 Novel Coronavirus (2019-
nCoV)
Responsibilities:
- The clinician should decide necessity for collection of clinical specimens for laboratory testing of 2019-nCoV only after following the case definition as given by the health authorities, Government of India.
- Appropriate clinical sample need to be collected by laboratory personnel/ health care worker trained in specimen collection in presence of a clinician.
- By following all biosafety precautions and using personal protective equipment (PPEs), clinical samples need to be sent to the designated laboratory (ICMR-NIV, Pune) by following standard triple packaging.
Selection of patient:
Any person who presents with Severe Acute Respiratory Illness (SARI) AND any one of the following i.e. a history of travel from Wuhan, China in 14 days prior to symptoms onset; disease in healthcare worker working in an environment of SARI patients; unusual or unexpected clinical course, especially sudden deterioration despite appropriate treatment; should be urgently investigated. Updated case definition need to be followed as per MOHFW, Govt of India which is available on the website www.mohfw.gov.in
Specimen collection details:
(Adapted from the WHO guidelines on 2019-nCoV):
| Specimen type | Collection materials | Transport to laboratory |
Storage till testing |
Comment |
| Nasopharyngeal and oropharyngeal swab | Dacron or
polyester flocked swabs* |
4 °C | ≤5 days: 4 °C >5 days: -70 °C | The nasopharyngeal and oropharyngeal swabs should be placed in the same tube to increase the viral load. |
| Bronchoalveolar lavage | sterile container* | 4 °C | ≤48 hours: 4 °C >48 hours: –70 °C | There may be some dilution of pathogen, but still a worthwhile specimen |
| Tracheal aspirate, nasopharyngeal aspirate or nasal wash | sterile container* | 4 °C | ≤48 hours: 4 °C >48 hours: –70 °C | Not applicable |
| Sputum | sterile container | 4 °C | ≤48 hours: 4 °C >48 hours: –70 °C | Ensure the material is from the lower respiratory tract |
| Tissue from biopsy or autopsy including from lung | sterile container with saline | 4 °C | ≤24 hours: 4 °C >24 hours: –70 °C | Autopsy sample collection preferably to be avoided |
| Serum (2 samples – acute and convalescent) | Serum separator tubes (adults: collect 3-5 ml whole blood) | 4 °C | ≤5 days: 4 °C >5 days: –70 °C | Collect paired samples:
|
*For transport of samples for viral detection, use VTM (viral transport medium) containing antifungal and antibiotic supplements. Avoid repeated freezing and thawing of specimens.
Specimen labelling and processing:
- Personal protective equipment (apron, hand gloves, face shield, N95 Masks etc.) need to be used and all biosafety precautions should be followed so as to protect individuals and the environment.
- Proper labelling (name/age/gender/specimen ID) need to be done on specimen container and other details of sender (name/address/phone number) on the outer container by mentioning “To be tested for2019-nCoV”
- For any queries, the nodal officer from ICMR-NIV Pune (Dr Yogesh K.Gurav, Scientist E) may be contacted (Phone 020-26006290/ 26006390; Email: gurav.yk@gmail.com/gurav.yk@gov.in) and need to be informed in advance
before sending specimens to ICMR-NIV, Pune.
Requirements for Clinical Samples Collection, Packaging and Transport
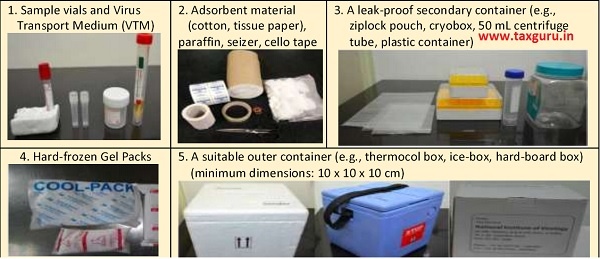
Procedure for Specimen Packaging and Transport

Documents to accompany:
1) Packaging list/proforma Invoice 2) Air way bill (for air transport) (to be prepared by sender or shipper) 3) Value equivalence document (for road/rail/sea transport) [ Note: 1. A vaccine-carrier/ice-box can also be used as an outer container 2. The minimum dimensions of the outer container should be 10 x 10 x 10 cm (length x width x height)]
Routing of samples:
- Clinical specimens, official documents and Specimen request forms for testing of 2019-nCoV need to be sent to the ICMR-NIV address (The Director, ICMR-National Institute of Virology, 20-A, Dr Ambedkar Road, Pune, Maharashtra, Pin: 4110001).
- For shipment-related queries/information, kindly contact Dr Sumit Bharadwaj (Scientist B, Influenza Group) on email: sumitduttbhardwaj@gmail.com, phone 020-26006290/26006390




